17 December 2021
Science and scenarios: agent-based models support decisions around COVID-19
Written by Jason Thompson, Associate Professor, University of Melbourne
For the last 18 months, The University of Melbourne’s Transport, Health and Urban Design Research Laboratory has been working feverishly alongside colleagues from across the University and beyond, to bring together data sources and methods that can assist decision-makers gain insight into the mechanisms driving infections, hospitalisations, and severe illness associated with COVID-19 within the Victorian and Australian community.
In this blog post, we’d like to give you just a small taste of these efforts, and also point readers to additional resources generated by our colleagues that may be of interest.
But first, let’s go back to the beginning.
In March 2020 there were no vaccines and no bespoke policy models available to Government, to assist them think through the options they had available to control COVID-19-related infection rates, hospitalisations and deaths in the Australian community.
Sure, there were epidemiological models, but there weren’t any policy models that could react dynamically to thresholds that decision-makers might consider reasonable.
Using agent-based models (ABMs), that’s what we set out to provide.
Benefitted by our relative geographic isolation, Australia had: 1) the advantage of being able to watch what was evolving across the rest of the world; 2) the ability and political willingness to close borders and mandate quarantine for international arrivals; and 3) a desire to achieve and maintain extremely low levels of virus circulation until a vaccine was available.
During the midst of a serious outbreak in mid-2021, the Department of Health (DoH) in Victoria used our agent-based model to assist them in thinking through their strategy for re-opening.
The model was rebuilt and co-designed with the DoH to reflect specifically Victorian conditions, including incorporating departmental advice and evidence on case numbers, current contact tracing performance, social restrictions and policy settings, community adherence to those policy settings and their impact on virus transmission.
The patterns observable in the model showed estimated disease progression through a simulated society resulting from either unmitigated spread or in response to staged social/physical distancing, or prophylactic technical or equipment adoption measures.
It included settings related to track and tracing apps, mask-wearing, school attendance policies and other related economic and social restrictions enacted and/or lifted over time. The policy model worked successfully as a decision support tool to aid the development of evidence-based policy and ultimately proved to be very accurate in estimating when Victoria might reach local elimination.
Since that time, the model has evolved dramatically. Now hosted on the University of Melbourne’s supercomputer, it can easily ingest new information about variant characteristics, vaccine effectiveness, as well as the effect of many more non-pharmaceutical interventions available in the armoury of public health officials and governments.
It is also available online in an interactive version. It is a forward-thinking, data driven and validated tool that has been of great assistance and great value to decision-makers.
Since its original publication, it has been joined by similar agent-based modelling conceptualisations from our colleagues in The Australian Covid-19 Modelling Initiative (AUSCMI) such as the Burnet Institute, University of Sydney, and University of Western Australia. Together, members of AUSCMI act to share modelling information, methods, data and techniques that can drive insights.
Our recently released pre-print manuscript on incorporating these modelling efforts into policy-making, emphasises the lessons we and others across Australia and the world have learned along the way.
But now that Australia has given up on ‘COVID-zero’ and moved into a phase of ‘living with the virus’, we face different threats.
Australia has achieved extremely high vaccination rates, reaching ~90% of the over-12 population in some states – especially those that have experienced the most severe lockdowns and social restrictions. But we are now no longer playing out longer-term static scenarios of what might be in the future, but what the more immediate dangers are for overwhelming the hospital system. Infections are one thing, but their translation into severe illness is another and this is now the main game.
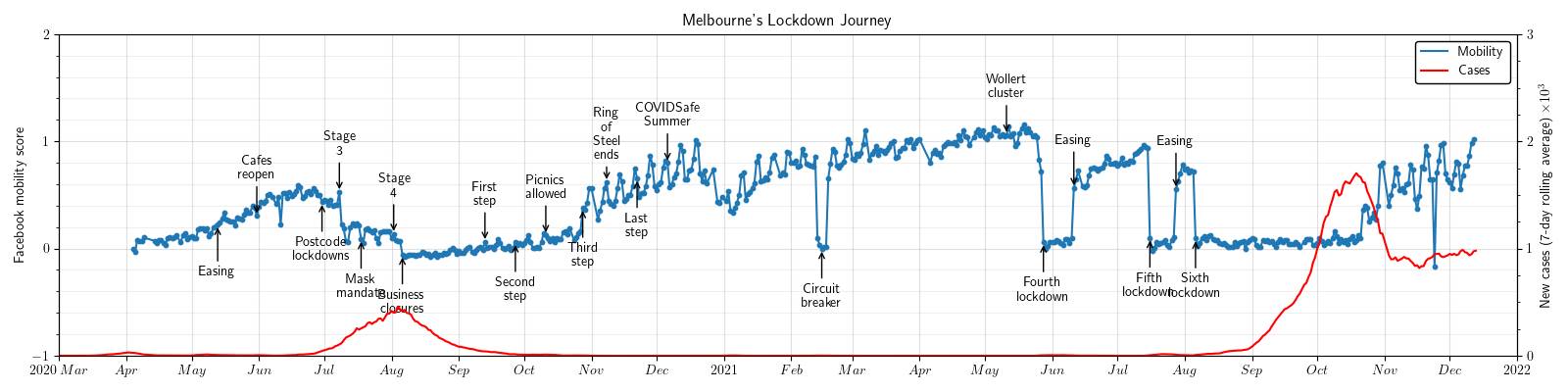
To this end, we have seen a shift from scenario modelling to data-driven, ‘nowcasting’ models. These nowcasting models enable health system planners to not only understand what the pressures on hospital systems might be across the state, but also within local government areas and health system catchment areas. They marry up-to-date epidemiological data, Facebook and Google mobility data, official data on health system access by area, demographic data, and up-to-date infection data, to estimate not only the number of expected infections across the community, but where they might occur, and which hospitals are likely to experience the greatest pressure.
This additional level of granularity helps everyone to understand not only what is going on in the system, but why.
National nowcasting coordinated by The Doherty Institute for Infection and Immunity and collected across different institutions in Australia, are very important for painting a national picture and importantly, have adopted a ‘many models’ approach to generated state-by-state estimates.
As COVID-19 evolves, so do the computational and data-driven methods that we at the University of Melbourne try to use, to keep up with its development. The modelling community has learned much in the past 18 months, especially in relation to the use of data-driven methods and the adoption of computational models for assisting decision-makers make better science-based (or at least science-informed) policy decisions.
Additional data is available at: https://rsbyrne.github.io/mobility-aus/